Updates to the Merit-based Incentive Payment System (MIPS) for 2020 include increasing the performance threshold to 45 points from the 30-point threshold for 2019 and finalizing the performance category weights, which are unchanged from 2019.
“Our approach for the 2020 Performance period is to maintain many of the requirements from the 2019 Performance period, while providing some needed updates to both the MIPS and Advanced [Alternative Payment Model] tracks to continue reducing burden, respond to feedback that we have heard from clinicians and stakeholders, and align with statutory requirements,” according to the Centers for Medicare & Medicaid Services (CMS) in its 2020 Quality Payment Program Final Rule Overview Fact Sheet.
MIPS is a system for value-based reimbursement under the Quality Payment Program, with the goal of promoting ongoing improvement and innovation to clinical activities. MIPS-eligible clinicians must meet objectives in 4 performance categories: (1) quality, (2) cost, (3) improvement activities, and (4) promoting interoperability (formerly known as the advancing care information performance category).
- For the quality performance category, clinicians pick the 6 measures of performance that best fit their practice.
- Cost refers to the cost of care provided as calculated by CMS based on the Medicare claims. MIPS uses cost measures to gauge the total cost of care during the year or during a hospital stay.
- Improvement activities refers to an inventory of activities that assess how clinicians improve their care processes, enhance patient engagement in care, and increase access to care. Clinicians choose the activities appropriate to their practice from categories such as enhancing care coordination, patient and clinician shared decision-making, and expansion of practice access.
- Promoting interoperability focuses on patient engagement and the electronic exchange of health information using certified electronic health record technology.
Performance in each category is weighted and used to calculate a final score from 0 to 100. The final score determines payment adjustment for the clinician. For 2020, which equates to the 2022 payment year, clinicians with final scores >45 will receive a positive payment adjustment. The performance category weights are as follows:
- Quality performance category is weighted at 45%;
- Cost performance category is weighted at 15%;
- Improvement activities performance category is weighted at 15%; and
- Promoting interoperability performance category is weighted at 25%.
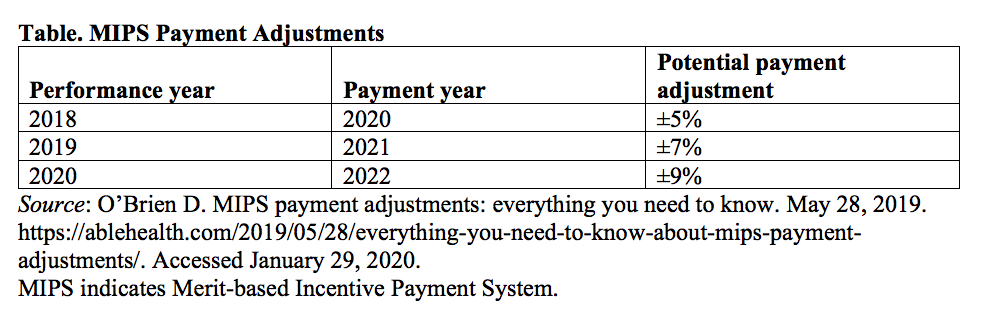
Payment adjustments are based on performance from 2 years prior. Depending on their scores, providers may receive bonus payments or be penalized. The maximum floor and ceiling for these payment adjustments have been increasing, and in the 2020 performance year, the risk corridor is ±9% (Table).
Exceptional performers that meet the additional performance threshold could receive an additional positive payment adjustment of up to 10%. The exceptional performance threshold for the 2020 performance period has been set at 85, an increase of 10 points compared with 2019. CMS has also finalized the performance threshold for the 2021 performance period at 60 points, and the additional performance threshold for exceptional performance will be 85 points (the same as 2020).
A new participation framework for MIPS that would begin with the 2021 performance period is the MIPS Value Pathways (MVPs). “We recognize stakeholder concerns about this timeline and are committed to a smooth transition to the MVPs that does not immediately eliminate the current MIPS framework,” wrote the CMS in their 2020 Final Rule Fact Sheet. “We will continue to engage with stakeholders to co-develop MVPs, to align with our goal of moving away from siloed performance category activities and measures and moving towards a set of measure options more relevant to a clinician’s scope of practice that is meaningful to patient care.”
The goal of these changes is to improve value, reduce burden, and remove barriers to participation in alternative payment models.