Barnes-Jewish Hospital in St. Louis, Missouri, is affiliated with the Siteman Cancer Center and Washington University School of Medicine. Barnes-Jewish Hospital has made the US News & World Report list of the 100 best hospitals in the United State for the past 21 years. It is the only hospital in St. Louis and the state of Missouri to have this designation. The hospital attracts some of the nation’s top doctors, is known for nursing excellence and the use of outcome and quality measures, and features the latest technology and research.
Sara K. Butler, PharmD, BCPS, BCOP, Clinical Pharmacist, Medical Oncology Clinical Supervisor, PGY2 Oncology Residency Program Director at Barnes-Jewish Hospital, talks about some of the programs at her institution and changes in the field of oncology.
What is your job description?
Sara Butler (SB): I am a clinical oncology pharmacist at Barnes-Jewish Hospital, working mainly with patients who have solid tumors or lymphoma. My job requires frequent collaboration with oncologists and medical residents about how to care for patients. Many of the patients I see are admitted for symptom management and complications of cancer therapy. I make recommendations based on their specific symptoms and the types of therapy they are receiving.
For example, if a patient with newly diagnosed colon cancer has significant peripheral neuropathy, I would recommend FOLFIRI rather than FOLFOX, because FOLFIRI does not exacerbate peripheral neuropathy since it does not contain oxaliplatin.
What is the approach to patient care at Barnes-Jewish Hospital?
SB: Barnes-Jewish Hospital is affiliated with Siteman Cancer Center—a National Cancer Institute–designated comprehensive cancer center—and Washington University in St. Louis, Missouri. Our approach to patient care is collaborative and incorporates teamwork from several types of specialists, including physicians, pharmacists, nurses, nurse practitioners, dietitians, physical therapists, and social workers.
How does this translate to improved patient care?
SB: The team approach provides different perspectives and addresses medical and nonmedical issues, so that patient management is more holistic.
What is exciting to you in the field of oncology?
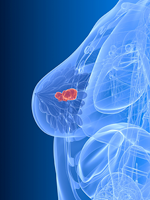
SB: The shift to targeted therapy over the past decade is a major advance. We’ve known for many years that receptors and pathways are important in the development and proliferation of cancer but we were unable to exploit these targets. In the era of targeted therapy, we now have many [treatments] specific to different cancer types. For example, in melanoma we have immunotherapy and other newer drugs that are being used in combination to extend the lives of patients. Other well-known examples are the multitargeted tyrosine kinase inhibitors for chronic myeloid leukemia, trastuzumab as well as newer drugs that target the HER2 receptor in HER2-positive breast cancer, and crizotinib for ALK-positive non–small cell lung cancer.
How has the role of the oncology pharmacist changed over the past
5 to 10 years?
SB: With conventional chemotherapy, we had to manage adverse events like nausea, vomiting, diarrhea, alopecia, and peripheral neuropathy, but targeted therapies have distinct side effect profiles. We have had to extend our knowledge and clinical experience to manage new symptoms associated with specific targeted therapies; for example, the immune effects of ipilimumab in patients with myeloma include autoimmune colitis or inflammation of other organ systems.
In the past, the oncology pharmacist didn’t have to manage these types of effects, which are specific to the drug. We need to learn whether to stop the drug, put it on hold, or continue treatment when adverse effects occur with targeted therapy. It can be challenging to keep on top of specific pathways and potential adverse effects.
What inspired you to become an oncology pharmacist?
SB: My inspiration was 2-fold: a family member with cancer and a fourth-year clinical rotation in oncology at pharmacy school. I was drawn to the field because I enjoy working with patients and find it rewarding to talk to patients who may be highly anxious about their therapy and to reassure them about side effects and the ability to manage them. On the inpatient side at our hospital, a clinical pharmacist is assigned to every inpatient, and we augment the education that nurses provide.
What advice would you give to a pharmacist just entering the field?
SB: I would say to keep an open mind and to look for opportunities on the inpatient and outpatient sides where you will be collaborating with physicians. The multidisciplinary approach is rewarding, and now pharmacy schools are increasing the number of oncology residency programs. Oncology is a high-cost area, and the expertise of pharmacists can help provide care efficiently and reduce inappropriate care.
If you weren’t a pharmacist, what would you be doing?
SB: I have always wanted to work in the medical field. Working in my hometown pharmacy during a summer when I was in college clinched my decision to become a pharmacist. Even though some patients may not survive, it is uplifting to be able to make patients feel better while they are undergoing treatment for their disease.